Cholinergic Drug
Cholinergic neurons
- primarily found within parasympathetic system
- sympathetic innervation of sweat glands
- blood vessels in skeletal muscle
Content:
2. Two types of cholinergic receptors
3. Drug--Cholinergic agonists
a. Direct acting cholinergic agonists
b. Indirect acting agonists reversible
Ease the symptoms of Alzheimer's disease
c. Indirect acting irreversible
4. Drug--Cholinergic antagonists
a. Antimuscarinic agents (anticholinergic drugs)
b. Ganglionic blockers
c. Neuromuscular blockers
ci. Nondepolarizing agents
cii. Depolarizing agents
5. Reference
1. Cholinergic neurotransmission
i. Choline molecule is transported into the neuron by energy and sodium dependent transport system. Once inside, choline reacts with Acetyl coenzyme A (AcCoA) to form Acetylcholine. The enzyme responsible for catalyzing this reaction is Choline Acetyltransferase.
ii. Acetylcholine gets transported into presynaptic vesicle where it's protected from degradation.
iii. The action potential causes the voltage-sensitive calcium channels to open. Thus allowing calcium to enter the axon. This leads to the fusion of the vesicle with the membrane and release of the acetylcholine from the terminal.
iv. Acetylcholine binds to postsynaptic receptor which leads to cholinergic response. Acetylcholine also binds to presynaptic receptors and inhibit the release of more acetylcholine. This serves as a negative feedback loop.
v. The enzyme called acetylcholinesterase, terminates acetylcholine function at the synaptic cleft by breaking it down to acetate and choline.
vi. The free choline is taken up again by the presynaptic neuron and the whole cycle gets repeated
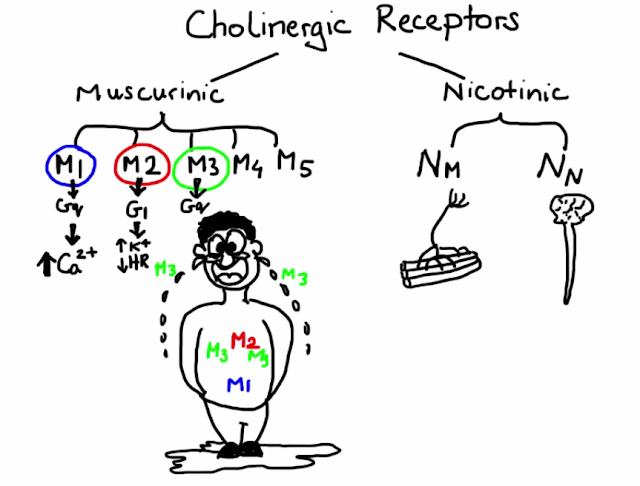
2. Two types of cholinergic receptors
- M1: Gastric glands
- Gq: increase in intracellular levels of calcium
- M2: Cardiac cells
- Gi: opening of potassium channels → hyperpolarization → reduction of heart rate
- M3:
- Smooth muscle in the eye, lungs, digestive tract
- Exocrine glands such as sweat and salivary
- Gq: increase in intracellular levels of calcium
- M4
- M5
- when acetylcholine binds to them these receptors, will undergo conformational change that allows sodium ions to flow into the cells.
- Nm: found on neuromuscular junction
- responsible for muscle contraction
- Nn: found in the central nervous system & autonomic ganglia
- involved in transmission of cholinergic signals
3. Drug--Cholinergic agonists
Three groups: Direct acting, Indirect acting reversible, Indirect acting irreversible
a. Direct acting cholinergic agonists
simply mimic the effects of acetylcholine by binding to either muscarinic or nicotinic receptors
i. Acetylcholine
- Problem: Clinical use is very limited
- produces nonspecific cholinergic effects
- rapidly inactivated by cholinesterases
- Side effect:
- decreases cardiac output and heart rate
- decreases blood pressure
- increases GI activity
- Usage: ophthalmic solution
- used to produce miosis during eye surgery
ii. Carbachol
- Problem: Limited therapeutic use
- structurally similar to acetylcholine
- effectively mimics effects of acetylcholine
- Pros: Long duration of action
- not very susceptible to acetylcholinesterases
- Usage: used only locally to constrict pupil during eye surgery and to decrease intraocular pressure
iii. Pilocarpine
- Usage: treating acute glaucoma attack
- acts on smooth muscle of the eye to constrict the pupil
- increases aqueous outflow which results in rapid drop in intraocular pressure
iv. Bethanechol
- Given orally or subcutaneously
- Usage: treat urinary retention or to treat gastrointestinal lack of muscular tone
- selectively stimulates urinary and gastrointestinal tract
- binding to acetylcholinesterase enzyme that catalyzes breakdown of acetylcholine
- results in buildup of acetylcholine in the synaptic cleft and corresponding effects
b. Indirect acting agonists reversible
i. Edrophonium
- reversibly binds to acetylcholineesterase
- very short duration of action 👉 about 10 to 20 minutes
- Usage: diagnosis of myasthenia gravis
- myasthenia gravis is a neuromuscular disease which is caused by antibodies that block acetylcholine receptors which leads to muscle weakness
- administered to a patient with myasthenia gravis 👉 rapid increase in muscle strength
ii. Physostigmine
- stimulates both nicotinic and muscarinic receptors
- intermediate acting agent: duration of action of about 30 minutes to 2 hours
- Usage: overdoses of anticholinergic drugs such as Atropine
iii. Neostigmine
- intermediate acting agent
- unlike Physostigmine its structure is more polar
- × absorb well from the GI tract
- × enter the CNS
- Usage: symptoms of myasthenia gravis
- stimulate bladder and GI tract
- reverse the effects of anesthesia from neuromuscular blocking agents
iv. Pyridostigmine
similar to Neostigmine
Side effect of Indirect acting agonists reversible
due to overstimulation of cholinergic receptors---"DUMBBELS"
sign of Organophosphate poisoining
- Diarrhea
- Urination
- Miosis / muscle weakness
- Bronchorrhea
- Bradycardia
- Emesis
- Lacrimation
- Salivation
Ease the symptoms of Alzheimer's disease
Function: enhance cholinergic effects and lead to improved cognitive function
*none of these agents can stop the progression of Alzheimer's disease
Drug: Donepezil, Rivastigmine & Galantamine
c. Indirect acting irreversible
- many of these drugs are extremely toxic
- were developed by the military as nerve agents
- eg, sarin gas
i. Echothiophate
- forms covalent bonds with acetylcholinesterase 👉 very strong cholinergic stimulation
- Usage: treatment of open-angle glaucoma
4. Drug--Cholinergic antagonists
Three groups: Antimuscarinic agents, Ganglionic blockers, Neuromuscular blockers
a. Antimuscarinic agents (anticholinergic drugs)
Block muscarinic receptors 👉 causing inhibition of muscarinic functions
i. Atropine
- Primary sites of actions: Eye, GI tract, Heart, Salivary, Sweat and Lacrimal glands
- Antimuscarinic activity of Atropine in the eye
- relaxation of ciliary muscle, cause
- dilation of the pupil (Mydriasis)
- inability to focus visually (Cycloplegia)
- Unresponsiveness to light
- Usage: before an eye exam or eye surgery
- treat certain inflammatory conditions of the eye
- Long duration of action
- other antimuscarinic agents such as Cyclopentolate and Tropicamide are preferred over Atropine
- Duration of produce mydriasis: last for days
- Cyclopentolate and Tropicamide: lasts for hours
- blocks M3 receptors in GI tract
- reduction of GI motility from stomach to colon
- prolonged gastric emptying & lengthen intestinal transit time
- block M2 receptors on the SA node and AV node (at higher doses)
- produces tachycardia heart rate may increase by as much as 30 to 40 beats per minute
- blocking muscarinic receptors on salivary sweat and lacrimal glands
- produces dry mouth dry skin and ultimately causes body temperature to rise
ii. Scopolamine
One of the most effective medications used for prevention of motion sickness and post-operative nausea and vomiting as it unlike Atropine has a much greater effect on the CNS as well as longer duration of action.
Available in a patch formulation that provides effects lasting up to three days
iii. Ipratropium and Tiotropium
block muscarinic acetylcholine receptors without specificity for subtypes
- → decreased contractility of smooth muscle in the lungs
- → bronchodilation and reduction of mucus secretion
Usage:
- inhalation for maintenance treatment of bronchospasms in patients with COPD Ipratropium
- treatment of rhinorrhea which is runny nose
- nasal spray formulation
Difference between Ipratropium and Tiotropium
Tiotropium is a long-acting agent that is dosed once daily
Ipratropium is a short-acting agent that typically requires up to four times daily dosing
iv. Tolterodine, Darifenacin, Solifenacin, Oxybutynin, Trospium and Fesoterodine
- Usage: treatment of overreactive bladder
- varying selectivity for the M3 receptor, which is the main receptor involved in bladder function
v. Benztropine and Trihexyphenidyl
- muscarinic blockers
- Usage: treatment of Parkinson-like disorders
- suppress central cholinergic activity
ABCDs
- A: Agitation
- B: Blurred vision
- C: Constipation and Confusion
- D: Dry mouth
- s: stasis of urine and sweating
b. Ganglionic blockers
i. Nicotine
- Although Nicotine is a cholinergic agonist, it is also considered a functional antagonist because of its ability to stimulate and then block cholinergic function
- acts on the nicotinic receptors of both parasympathetic and sympathetic autonomic ganglia
- increased release of neurotransmitters such as dopamine, serotonin and norepinephrine
- Nicotine is a nonselective it stimulates and later depresses autonomic ganglia
- eg, Nicotine stimulates CNS which at high enough doses can lead to convulsions and then it depresses CNS which can lead to respiratory paralysis
- by stimulating adrenal medulla and sympathetic ganglia, nicotine increases blood pressure and heart rate
- at higher doses it can cause blood pressure to fall
- in GI system, nicotine increases the motility which can lead to nausea and vomiting
- Cons: addiction due to CNS stimulation that produces increased alertness and surge of well-being
c. Neuromuscular blockers
Block the cholinergic transmission between motor nerve endings and nicotinic receptors on the skeletal muscle
Nerve ending meets the skeletal muscle fiber
- nicotinic receptors to which acetylcholine can bind and induce their opening
- opening of these channels let sodium ions to enter the muscle fiber
- trigger muscular action potential
- the potential travels along the surface of sarcolemma which is the excitable membrane that surrounds those cylindrical structures known as myofibrils
- then the action potential travels through T-tubule system which penetrates into the fiber
- the arrival of action potential causes calcium to be released from the sarcoplasmic reticulum
- muscle contraction
ci. Nondepolarizing agents
- Competitive antagonists: bind to acetylcholine receptors but they don't induce ion channel opening
- prevent depolarization of the muscle cell membrane and thus effectively inhibit muscle contraction
- Usage:
- facilitate mechanical ventilation and tracheal intubation
- increase muscle relaxation during surgery which allows for lower doses of general anesthetics
- Must be injected
- not absorbed from GI
- Time to onset of action: usually less than two minutes
- Once administered,
- these agents paralyze small fast contracting muscle first, eg, eyes, face, fingers
- then larger muscles of neck trunk and limbs
- lastly diaphragm
- Muscles recover in the reverse manner
Choice of an agent typically depends on the desired onset and duration of the muscle relaxation
Clinical duration: a time measured from administration to recovery of 25% of baseline muscle strength
- Cisatracurium: 90 minutes
- Pancuronium: 90 minutes
- Rocuronium: 40 minutes
- Vecuronium: 40 minutes
- Atracurium: 40 minutes
Side effects
1. Atracurium
- causes histamine release which results in
- fall in blood pressure
- flushing
- bronchoconstriction
- toxic metabolite---laudanosine
- provoke seizures especially in patients with impaired renal function
*Hence, Atracurium has been largely replaced by its isomer Cisatracurium
2. Cisatracurium
- less likely to produce the same adverse effects
- as metabolism is independent of hepatic or renal function
*Cisatracurium is often used in patients with multi-organ failure
3. Vecuronium and Rocuronium
- safe and have minimal side effects
- metabolized by liver so their action may be prolonged in patients with hepatic dysfunction
4. Pancuronium
- increase in heart rate
- Pancuronium is excreted unchanged in urine
cii. Depolarizing agents
Act as acetylcholine receptor agonists, they mimic the acetylcholine.
However they are much more resistant to degradation by acetylcholinesterase and therefore produce persistent depolarization.
i. Succinylcholine
- binds to the nicotinic receptor
- unlike the nondepolarizing agents, it actually causes the sodium channel to open which results in membrane depolarization
- Usage:
- facilitate rapid sequence endotracheal intubation in critically ill patients
- rapid onset of action
- provide adequate muscle relaxation during electroconvulsive therapy (intravenous)
- complete muscle relaxation: within one minute
- the effects typically last up to ten minutes
Action
Phase-1 block
because Succinylcholine is resistant to acetylcholinesterase, it causes prolonged depolarization which leads to a transient fasciculations and finally flaccid paralysis.
Eventually sodium channel closes and membrane repolarizes. However due to continued stimulation by Succinylcholine the receptor becomes desensitized to acetylcholine. Thus, preventing formation of further action potentials.
Adverse effects of Succinylcholine
- Prolonged Apnea
- due to rapid redistribution and hydrolysis by plasma pseudocholinesterase
- patients deficient in plasma pseudocholinesterase or patients who have genetic variation of this enzyme
- Hyperkalemia
- prolonged depolarization caused by Succinylcholine, leads to continued flow of potassium into the extracellular fluid
*In patients with normal potassium levels this is usually not a big issue
However in those with elevated potassium levels, eg. due to burns or large tissue damage, can cause serious EKG changes, and even in severe cases asystole.
- Malignant hyperthermia
- In genetically susceptible patients, Succinylcholine can trigger rare and potentially fatal condition
- Symptoms of malignant hyperthermia:
- severe muscle contractions
- dangerously high body temperature---43 degrees Celsius
5. Reference
https://youtu.be/r-gJaMoMon
https://youtu.be/cp_CZpCBVpk
NEXT:
PREVIOUS:








Comments
Post a Comment