Hypertension
or high blood pressure is a quite common disorder affecting many people who typically don't even notice any symptoms.
Content:
2. Antihypertensive drugs
a. Alpha-1 blockers
b. Selective beta blockers
c. Non-selective beta blockers
d. Centrally acting adrenergic drugs
e. Calcium channel blockers
f. Diuretics
g. renin-angiotensin-aldosterone system
h. Bosentan
i. Fenoldopam
j. Sodium Nitroprusside and Nitroglycerin
k. Hydralazine & Minoxidil
3. Reference
1. Blood pressure regulation
Blood pressure: The force or tension of blood pressing against the artery walls
- maintained by
- contraction of the left ventricle
- systemic vascular resistance elasticity of the arterial walls
- blood volume
Formula: blood pressure is a product of cardiac output and systemic vascular resistance
Arterial blood pressure is regulated by pressure sensitive neurons called baroreceptors
- Baroreceptors located in the aortic arch and carotid sinuses
- If blood pressure falls too low, baroreceptors can send signals to the adrenal medulla
- causing release of catecholamines
- thus increase in sympathetic activity through activation of alpha and beta receptors
- activation of beta-1 receptors causes increase in heart rate and stroke volume
- increased cardiac output
- increase in blood pressure
- activation of alpha-1 receptors on smooth muscle causes vasoconstriction
- increase in vascular resistance
- leads to increase in blood pressure
Baroreceptors in the kidneys that respond to fall in blood pressure or reduction of blood flow (renin-angiotensin-aldosterone system)
- by releasing enzyme called renin
- renin secretion is also stimulated by sympathetic activation of beta-1 receptors in the kidneys
- renin is necessary for the production of angiotensin II
- angiotensin II is a very potent vasoconstrictor which constricts systemic blood vessels
- increasing peripheral resistance angiotensin II
- constricts renal blood vessels
- stimulates aldosterone secretion
- leads to sodium and water retention
- increased blood volume cardiac output
- increased blood pressure
2. Antihypertensive drugs
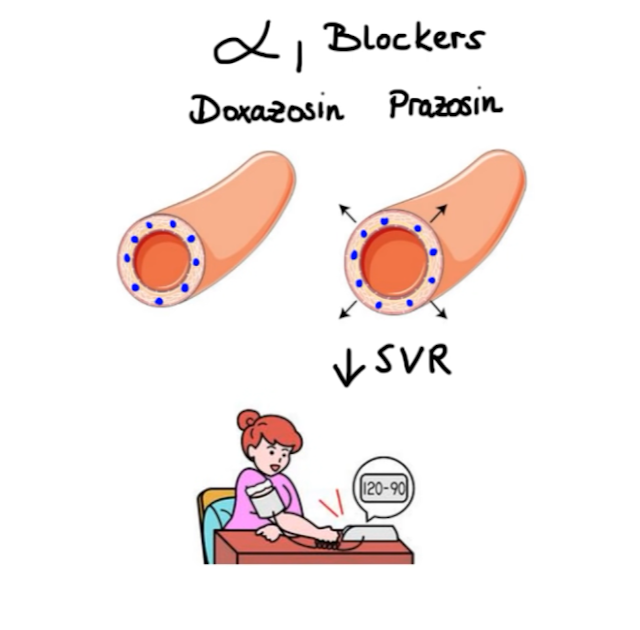
a. Alpha-1 blockers
Drug:
- Doxazosin
- Prazosin
- block alpha-1 receptors on the smooth muscle
- causing decrease in systemic vascular resistance
- decrease in blood pressure
b. Selective beta blockers
Drug:
- Atenolol
- Metoprolol
- selectively block beta-1 receptors on the heart
- decrease in cardiac output
- decrease in blood pressure
c. Non-selective beta blockers
Drug:
- Labetalol
- Carvedilol
- additionally block alpha-1 receptors
- simultaneously decrease vascular resistance
- beta blockers can inhibit beta-1 receptors present on the kidneys
- suppress release of renin, formation of angiotensin II and secretion of aldosterone
- decrease in systemic vascular resistance
- fall in blood pressure
d. Centrally acting adrenergic drugs
work by blocking sympathetic activity within the brain
Drug:
- Clonidine
- selectively stimulates presynaptic alpha-2 receptors
- providing negative feedback to reduce catecholamine production
- decrease in systemic vascular resistance and cardiac output
- decreased blood pressure
- Methyldopa
- lowers blood pressure through the same mechanism
- however unlike Clonidine it is not an agonist itself
- so first it must be converted to its active metabolite called methylnorepinephrine
e. Calcium channel blockers
divided into two main subclasses:
- dihydropyridines
- selectively inhibit L-type calcium channels in the vascular smooth muscle under normal conditions
- blocks the entry of calcium
- contraction is inhibited
- decreased resistance to blood flow
- lowering of blood pressure
- Normal: when calcium enters the smooth muscle cell
- cause contract which leads to increased vascular resistance
- increase in blood pressure
- Drug:
- Amlodipine
- Felodipine
- Nicardipine
- Nifedipine
- nondihydropyridines
- non selective inhibitors of L-type calcium channels
- blocking calcium channels on vascular smooth muscle and on cardiac cells (eg, SA node and AV node)
- leads to reduced myocardial contractility
- slower heart rate and slower conduction
- but do not significantly decrease cardiac output
- most likely because of the reflex tachycardia that occurs as a result of vasodilation
- Drug:
- Diltiazem
- Verapamil
Side effects of dihydropyridines
- dizziness
- headache
- flushing
- peripheral edema
- as related to systemic vasodilation
- gingival hyperplasia (swelling of gums)
Side-effects nondihydropyridines
- excessive bradycardia and cardiac conduction abnormalities
- Verapamil: constipation
- least selective calcium channel blocker can exert significant inhibition of calcium channels in the smooth muscle that lines the GI tract
f. Diuretics
- work by reducing reabsorption of sodium chloride in the kidneys
- leading to significant diuresis with less volume in the vascular space
- less blood returns to the heart
- cardiac output decreases
- decrease in blood pressure
- particularly in patients with volume-based hypertension and chronic kidney disease
- reduce reabsorption of sodium chloride in the kidneys
- but to a much smaller degree than loop diuretics
- leads to initial decrease in intravascular volume
- decrease in cardiac output
- lower blood pressure
- However the long term effects on blood volume are minimal and sustained
iii. potassium-sparing diuretics
Drug:
- Triamterene
- Spironolactone
- increase diuresis by
- interfering with the sodium potassium exchange in the kidneys
- blocking the actions of aldosterone
- often used in combination with loop and thiazide diuretics
- to reduce loss of potassium
g. renin-angiotensin-aldosterone system
Three pharmacological targets to reduce the activity of angiotensin II:
i. renin
- the enzyme responsible for conversion of angiotensinogen to precursor of angiotensin II
- Renin inhibitors which selectively inhibit this enzyme
- thus decreasing production of angiotensin II
- Drug: Aliskiren
ii. Angiotensin-converting enzyme
- responsible for conversion of angiotensin I to angiotensin II
- Target of ACE inhibitors
- inhibition of angiotensin-converting enzyme
- leads to decreased production of angiotensin II
- Make it different: lowering angiotensin II levels & also elevate bradykinin levels
- bradykinin is a peptide that causes blood vessels to dilate by stimulating the release of nitric oxide and prostacyclin
- however normally angiotensin-converting enzyme inactives bradykinin
- so it's inhibition leads to bradykinin induced vasodilation
- Drug:
- Benazepril
- Captopril
- Enalapril
- Lisinopril
- Quinapril
- Ramipri
iii. Angiotensin II receptors type 1 (AT1 receptors)
- responsible for most of the effects of angiotensin II, including
- vasoconstriction
- stimulation of aldosterone
- Target of angiotensin II receptor blockers (ARBs)
- work by
- block the production of angiotensin II or
- block its actions on the AT1 receptors
- decreased systemic vascular resistance but without significant changes in cardiac output
- Additionally, reduce the effects of angiotensin II on renal hemodynamics
- specifically angiotensin II constricts the efferent arteriole
- generating back pressure in the glomerulus
- lead to injury
- Hence, by reducing activity of angiotensin II
- improve renal blood flow
- reduce the risk of renal injury
- Drug:
- Candesartan
- Irbesartan
- Losartan
- Olmesartan
- Valsartan
Side effects
- hyperkalemia
- as suppress aldosterone release
- ACE inhibitors: dry cough or angioedema (life-threatening)
- due to increased levels of bradykinin and substance P
h. Bosentan
- competitive antagonist of a potent vasoconstrictor called endothelin-1
- act on endothelin-A and endothelin-B receptors located on pulmonary vascular cells
- by blocking the action of endothelin-1 on these receptors
- vasodilation
- decreases pulmonary vascular resistance
- choice for treatment of pulmonary hypertension
i. Fenoldopam
- selective dopamine-1 receptor agonist
- dopamine-1 receptors are located on the
- smooth muscle cells in the peripheral vasculature
- renal coronary cerebral
- mesenteric arteries
- by stimulating dopamine-1 receptors
- produces generalized arterial vasodilation
- leads to decreased peripheral resistance
- lower blood pressure
- Additionally, Fenoldopam inhibits tubular sodium reabsorption
- results in natriuresis and diuresis
- due to its rapid onset of action and short duration of action
- use for short-term management of severe hypertension
j. Sodium Nitroprusside and Nitroglycerin
- fast-acting agents that are also used for hypertensive emergency
- serve as
- a source of nitric oxide
- a potent peripheral vasodilator
k. Hydralazine & Minoxidil
- direct acting smooth muscle relaxants
- Hydralazine: mechanism of action that has not been entirely determined yet
- Minoxidil: works by stimulating opening of ATP-activated potassium channels in the smooth muscle
- leads to membrane stabilization making vasoconstriction less likely
- Both result:
- significantly decrease peripheral resistance
- also produce significant compensatory reflex---tachycardia and renin release
- typically administered in combination with a diuretic and a beta blocker
- topical application of Minoxidil: promotes hair growth
- so more often for treatment of baldness, rather than hypertension
3. Reference
https://youtu.be/V2sEay-E-Ro








Comments
Post a Comment